What's going on in the NHS?

The NHS marked its 75th anniversary in July 2023, meaning that most of us can’t remember a time when it didn’t exist. It’s been a constant source of discussion, both politically and in the media. We examine the data to discover what’s happening in the NHS as of August 2023.
Waiting times are still a key issue
NHS waiting times were an issue before COVID-19, and the increased demand that the pandemic placed on NHS services only made matters worse.
House of Commons Library Research
In July 2023, the House of Commons Library published research into demand, waiting times and performance for vital NHS services in England. Their research is stark, laying bare the severity of our health service’s current situation.
Waiting list for consultant-led treatment reaches 7.6m
As of June 2023, the waiting list for consultant-led treatment, often called “elective care”, reached 7.6 million patients in England. To put that into context, the population of England is only 56 million people, so that’s close to 14% of us awaiting treatment!
As can be seen by the chart below, while the growth of the waiting list accelerated due to the COVID-19 pandemic, it was already growing year on year, back to around 2012, and if past performance is anything to go by, we can expect it to keep growing.
The Government has announced measures such as greater use of private hospitals to help reduce this backlog, but many aren’t convinced this will solve the problem. The independent charity The Health Foundation stated they believe it’ll have “limited impact” based on a study they conducted earlier in the year.
Unfortunately for those living in England, the grim milestone of 8 million patients waiting isn’t far off and is likely a case of when not if.

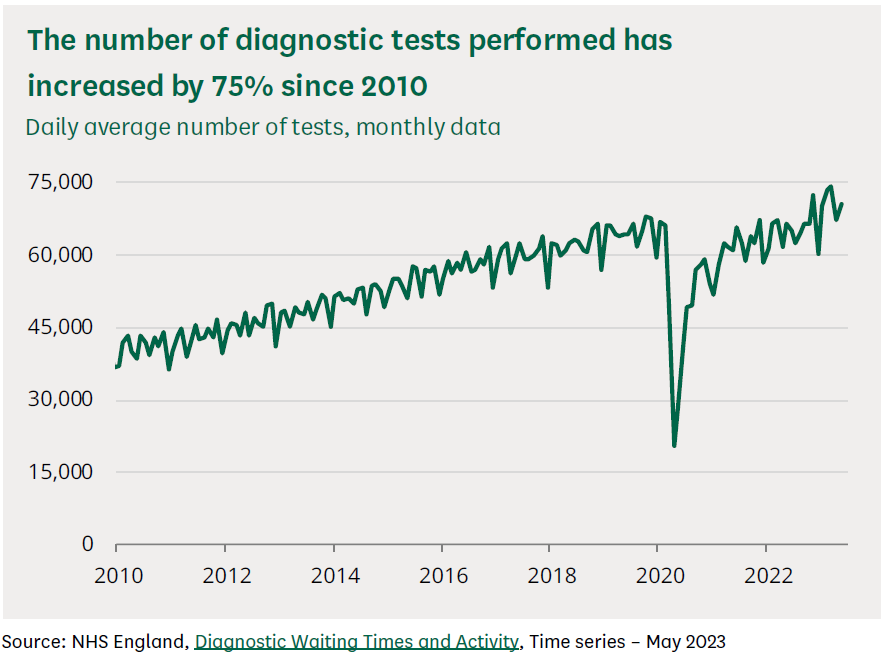
Demand for diagnostic tests at record levels
In 2019, before the Covid-19 pandemic, there were around 23.6 million diagnostic tests commissioned by the NHS in England. These tests include things like MRI and CT scans, as well as non-obstetric ultrasounds and numerous others.
The level of diagnostic testing reduced during the pandemic as the NHS focused on Covid-19. However, in recent months, the volume of tests has risen beyond pre-Covid levels.
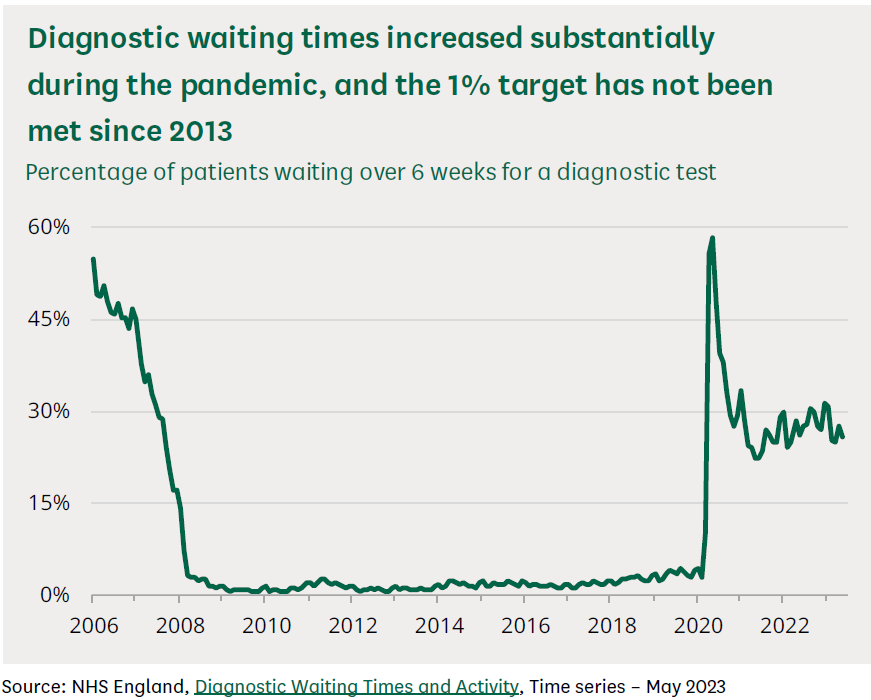
Six week wait target for diagnostic tests has not been met since 2013
When the NHS turned its focus to dealing with Covid-19, and reduced the number of diagnostic tests on offer, the percentage of people waiting longer than six weeks rocketed, far above the 1% target.
However, as can be seen from the chart below, while there has been some recovery, it’s still hovering between 25-30% of people having to wait longer than six weeks.
23,499 people waiting for cancer treatment for longer than 62 days (May 2023)
A lot of cancer diagnosis and treatment data focuses on waiting times after patients start a course of treatment, not on those still waiting for treatment to begin. There isn’t any formal, routinely published data on how many people are waiting for treatment and how big any backlog might be.
However, the House of Commons Library researchers have found that NHS England has started publishing “management information” showing the number of patients waiting over 62 days for treatment after an urgent GP referral with suspected cancer.
The chart below shows the number of people waiting more than 62 days but doesn’t include anyone waiting less than that time.
As you can see, there was a peak at the start of the pandemic but then a reduction up to around September 2021. Since then, the number of people waiting more than 62 days has fluctuated and remains stubbornly higher than pre-pandemic levels.
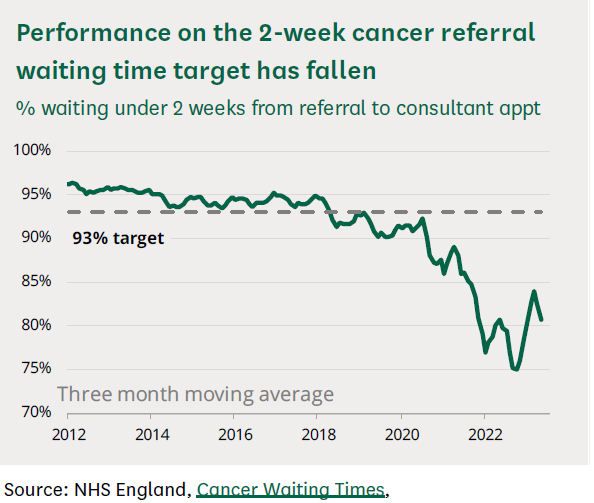
Government scraps 2-week cancer referral targets
The government has recently announced its intention to scrap the 2-week cancer referral target, which aimed for 93% of those referred urgently due to suspected cancer to be seen by a consultant within 14 days. That target hasn’t been met since early 2018 and will now be replaced by a new “Faster Diagnosis Standard“.
The Faster Diagnosis Standard targets that 75% of patients are told whether they do or don’t have cancer within 28 days, rather than just a consultation within 14.
If the targets are met, then it should lead to faster treatment. However, this new standard was introduced some 16 months ago and is yet to be achieved, although it came close to it at 73.5% in June 2023.
This resource from Cancer Research is handy if you want to see the current performance against the various targets. Updated monthly, it gives you a close-to-live view of what’s happening concerning Cancer in the NHS.

The junior doctors’ strike
Industrial action by junior NHS doctors seeking fairer pay and conditions is ongoing. The dispute relates to the most recent pay offer in 2022, which provided a below-inflation rise of 2%. A 2022 survey by the British Medical Association indicated that junior doctors were experiencing the impact of the cost of living crisis, with over 50% struggling to pay their bills and around 80% reducing the amount they spend on food and utilities.
Statistics from NHS England found that four days of strike action in August 2023 led to 61,200 appointments and procedures being rescheduled as over 23,000 NHS staff were away from work.
At this stage, further strike action remains a possibility. Senior NHS staff estimate that further action could mean rescheduled appointments will hit the 1 million mark.

Staff shortages
The summer of 2023 has proved to be one of the busiest in recent years, with NHS emergency services dealing with 4.42 million attendances during June and July, compared to 4.37 million during the same period in 2022. There were also record numbers of checks and diagnostic tests as staff worked to reduce waiting times.
However, this is happening against a backdrop of continued understaffing and increased stress among staff. Mixed teams, which include medical, nursing and other support staff, typically deliver medical care, so hospitals must have sufficient staff numbers to cover the workload adequately. In March 2023, there were 112,498 vacancies in England. Most of these were in nursing care, with over 40,000 vacant posts.
The BMA stated that this creates a risk of burnout amongst staff as they struggle to cover excessive workloads. Staff may take more time off sick or leave the profession altogether, causing a further drop in staff numbers.
The Government’s Autumn budget statement provided additional funding to support the NHS and social care services. It also promised a workforce plan to provide additional staff and fill existing vacancies over the next 5, 10 and 15 years.

An ageing population
We have an ageing population, with the number of people over 85 predicted to double in the next 25 years. Whilst many older people can live independently, research has found that demand for care has increased thanks to a rise in the number of over-75s with a long-term chronic condition. As we age, we’re also at greater risk of falls and needing emergency treatment.
A recent report from Age UK, a charity working with older people, raised concerns about the ability of the NHS and social care services to work together effectively to care for older people. They describe the current approach as being reactive rather than proactive. They also raise concerns about the care burden on family members and ‘the sandwich generation’, the people who are caring for their elderly parents and their children at the same time.
The solution will likely lie in multi-agency cooperation, more integrated services and greater funding to increase staffing levels and support unpaid family carers.

Growing pressure on GPs
Whilst GPs haven’t taken industrial action, general practice faces many of the same issues as the wider NHS. GPs are the first stop for most patients. However, the number of patients per GP has risen, impacting doctors’ ability to build long-term relationships with their patients. The average number of patients a full-time GP looks after is now 18.9% higher than in 2015.
Statistics show that there has been negligible growth in the number of full-time GPs over the past eight years. This is due to various factors, including falling recruitment and GPs changing their working hours to move towards part-time rather than full-time work.
The 2022 GP patient survey found that patient satisfaction was declining in terms of the availability of appointments and their overall experience. One of the most striking statistics relates to patients’ satisfaction with their ability to make an appointment. In 2021, 70.6% of patients had a good experience making an appointment; by 2022, that figure was down to 56.2%.

Virtual wards
The number of hospital beds in the UK has halved over the past 30 years. In the past few months, this has been accompanied by a rise in the number of virtual wards. The number of virtual beds stood at 9,713 at the end of July 2023, and there are plans to increase these numbers further by the end of September.
What is a virtual ward?
The idea behind virtual wards is that they will ease pressure on the NHS estate and allow NHS staff to manage patient care remotely. The idea is that staff can provide hospital treatment without the patient needing a hospital bed. There are daily reviews, and staff can offer home visits, prescribe medication and order tests or scans as necessary.
This type of treatment is still in its infancy. Research indicates that selecting the right patients is vital, as is developing a suitable multi-disciplinary team. This approach is unlikely to provide a quick and easy solution but could make a positive difference with the proper support.

New health campaigns and partnerships
Health education is vital in improving patient outcomes and reducing the burden on NHS services. One of the most recent campaigns has focused on teaching people to recognise the signs of a heart attack and when to call 999. Early treatment increases a patient’s chances of survival, but patients often ignore early indications.
There’s also a new partnership with Morrisons, who are putting cancer awareness labels into their own-brand underwear. The labels will include information on testicular cancer in boxer shorts and breast cancer in crop top bras to increase awareness and encourage self-examination.

Getting professional advice
The NHS continues to face significant challenges in attracting and retaining its workforce and coping with increased patient demand. Private healthcare and health insurance can provide an alternative to NHS care by offering virtual GP appointments, diagnostic tests and private surgery.
At myTribe, we offer guides and information to help you understand your options and make an informed choice about your healthcare. If you want to learn more about private medical insurance, contact us for a comparison quote. We’ll put you in touch with a high-quality, regulated broker to provide advice tailored to your circumstances.
Disclaimer: This information is general and what is best for you will depend on your personal circumstances. Please speak with a financial adviser or do your own research before making a decision.







