Should race/ethnicity variables should be used in developing clinical prediction algorithms?
That is the question a paper by Anirban Basu (2023) in Science Advances attempts to answer. A key assumption the article makes is that race is a social and not a biological construct. Basu justifies this assumption by stating that “the vast majority of genetic variation associated with race-specific traits exists within racial groups and not between them.”
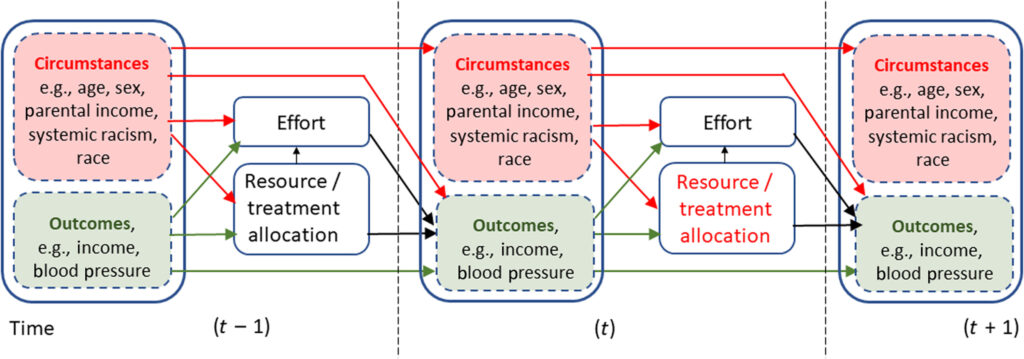
The study also uses an ‘equality of opportunity’ framework. This approach has been widely used in economics (see Roemer 2002, Becker 1971) as well as in other fields. Basically, in the EO framework, outcomes depend on individuals have circumstances (e.g., age, gender, race, parental income) that are largely outside of their control of individuals as well as their own efforts. There is inequality of opportunity whenever outcomes differ across circumstances when effort is held constant.
The Basu paper, however, notes that effort may not be a full choice variable as there may be barriers to individuals making efforts–particularly in the past–which could accumulate and change circumstance over time and result in worse health outcomes even with identical efforts in the current period. He writes:
…the dynamic health production functions for outcomes, which are the prediction targets, include the legacy effects of biological and nonbiological outcomes and current individual efforts. Several social determinants and systemic racism shape these efforts. When invoking E.O. [equality of opportunity], inequality of outcomes arising from (future) individual efforts should not be driving current prescriptive resource allocation at the individual level. This is because the opportunity to improve outcomes from baseline should be equally available to everyone, irrespective of whether anyone seizes those opportunities to produce better outcomes.
Graphically, the paper uses the dynamic framework below.
Basu concludes that whether race should be included in clinical prediction algorithms depends on the goal of the algorithm.
…in practical settings, failure to include race corrections will propagate systemic inequities and discrimination in any diagnostic model and specific prognostic models that inform decisions by invoking an ex ante compensation principle. In contrast, including race in prognostic models that inform resource allocations following an ex ante reward principle can compromise the equality of opportunities for patients from different races. In such settings, race is likely to proxy for differential efforts across these groups, which unobserved differential circumstances can shape. Even when race is not included, discrimination is likely to be part of any algorithms predicting future outcomes used to devise an ex-ante reward policy, although including race exacerbates this problem.
The article includes both formal derivations of cases when it is and is not acceptable to include race/ethnicity in a clinical algorithm depending on whether it is a diagnostic (current) or prognostic (future prediction) algorithm and whether the algorithm is used to identify current issues, or reward performance. For instance, CMS largely has not included race in value-based provider reimbursement since doing so would cause quality of care standards to vary by race; however CMS does track retrospectively differences in health outcomes across races to identify potential issues as a diagnostic tool, however. The paper also uses a simulation model to examine how the dynamics in the figure above can manifest itself when effort itself is differentially rewarded.
You can read the full paper here.







