Medicare-Eligible Workers Face a Dilemma
What You Need to Know
More workers are 65 or older.
They could stick with the employer plan.
For some a Medicare plan may be a bitter fit.
As fall approaches, many employers and their Medicare-eligible employees enter an important time: open enrollment.
This period allows individuals to assess both their employer’s 2025 benefit plans and Medicare’s enhanced options.
With significant Medicare improvements in 2025, this is an ideal moment to reassess coverage, as switching to Medicare may offer better benefits at a lower cost.
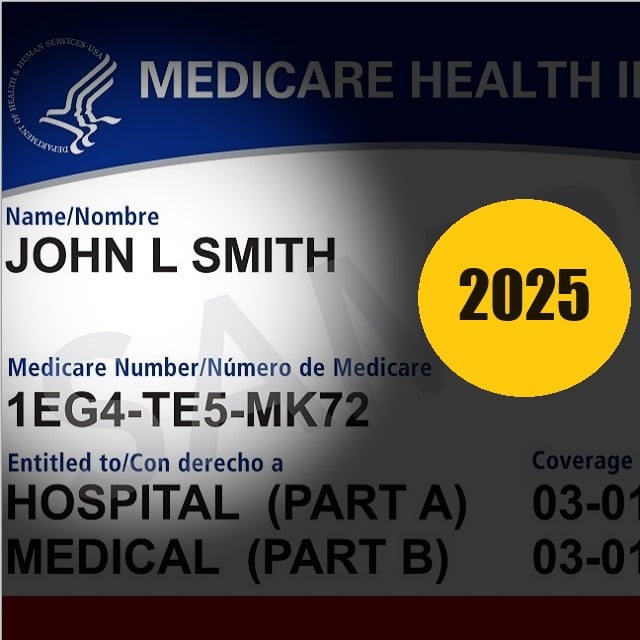
John, a 68-year-old warehouse manager with over 30 years of service, faced a decision: remain on his employer’s health plan or switch to Medicare? With rising premiums and increasing prescription costs for managing high blood pressure and cholesterol, John needed to carefully evaluate which option would best meet his health care and financial needs.
His situation reflects that of many Medicare-eligible employees during open enrollment.
The Choice in 2025
This open enrollment period presents an opportunity for Medicare-eligible employees to weigh their options.
With Medicare offering enhancements, and employer plans adjusting costs and coverage for the next year, the decision isn’t always straightforward.
Let’s break down the key considerations.
The Importance of Creditable Coverage
A critical factor for Medicare-eligible employees is whether their employer’s plan qualifies as “creditable coverage,” meaning it meets Medicare’s standards for prescription drug coverage.
In John’s case, his employer confirmed their plan was creditable, allowing him to delay Medicare enrollment without penalties.
However, employees without this confirmation could face higher costs when enrolling in Medicare later.
Employers should ensure that employees are informed about their plan’s creditable status, as failure to provide this information can lead to penalties and increased health care costs.
Medicare Improvements
Part D will cap out-of-pocket prescription drug expenses at $2,000 annually.
This was a major incentive for John, whose medication costs had been rising.
John explored Medicare largely due to the improvements coming in 2025, which present a unique opportunity for workers to reconsider their health care coverage.
Key changes include:
Lower prescription drug costs: Starting in 2025, Medicare, beneficiaries will have maximum out-of-pocket costs for their Part D drugs. They will not pay more than $2,000 per year.
Expanded drug coverage: In 2025, Part D will provide access to medications that were not previously covered. Medications like Mounjaro and Ozempic, which previously were not covered for weight loss, might be covered for other conditions like diabetes and cardiovascular diseases.






