Medicare Advantage May Face Big Plan Cuts, Price Hikes in 2025
What You Need to Know
Elevance talked about seeing pockets of very aggressive competition.
Humana posted a $540 million loss and says costs are running much higher than expected.
Humana adjusted for the new COVID surge and believes other factors are also driving up costs.
The Medicare Advantage program could go through huge upheaval in 2025, with the changes showing up in annual enrollment period plan menus Oct. 15, as voters are heading to the polls for the fall general elections.
Executives from Humana, a major Medicare Advantage plan and Medicare drug plan provider, said Thursday during a conference call with securities analysts that it believes that some competitors’ pricing has been unsustainably aggressive, new regulations are driving up costs, and that health care claim costs have been much higher than it had expected, even after adjusting for the new flu and COVID-19.
Humana will be “very intentional” about which markets it will serve in 2025, Humana CEO Bruce Broussard said.
“Looking to 2025, we are evaluating MA pricing actions,” Broussard said. “I look at next year as a year when I think the whole industry will possibly reprice.”
What it means: Clients who have Medicare Advantage plan coverage may have to change plans in 2025 or face significantly higher premiums.
Many health coverage advisors and their clients strongly prefer combining original Medicare with Medicare supplement, or Medigap, insurance, and it’s possible that problems in the Medicare Advantage market could lead to new insurer interest in the Medigap policy market.
Humana’s earnings: Humana talked about the Medicare Advantage plan market when going over results for the fourth quarter of 2023.
The company is reporting a $540 million net loss for the quarter on $26 billion in revenue, compared with an $18 million net loss on $22 billion in revenue for the fourth quarter of 2022.
The company ended the year providing or administering medical coverage for 17 million people, or about 1.3% fewer people than it was covering a year earlier.
Some of the net loss was due to $764 million in costs related to a decision to get out of the employer health coverage market.
Susan Diamond, Humana’s chief financial officer, said that Humana understood going into the fourth quarter that the new wave of COVID cases and other outbreaks of other respiratory diseases could drive up costs, and that the company had factored that into forecasts.
The effects of respiratory disease care turned out to be somewhat less than the company had feared.
Factors that Humana is analyzing include the effects of new Medicare Advantage plan benefits rules, a big influx of enrollees who have “aged into” Medicare, and the relatively high cost of covering age-ins.
Other factors that could increase costs are the effects of pandemic-related decreases in use of preventive and routine care in 2020 and early 2021 and the possibility that COVID may be affecting the odds of patients having other, seemingly unrelated conditions.
The list of challenges for plans also includes new Medicare marketing regulations; incoming restrictions on the preauthorization programs used to hold down unnecessary use of care; and a belief by some members of Congress that cutting the federal Medicare Advantage program spending is a good way to narrow the federal budget deficit or find spare cash to pay for other programs.
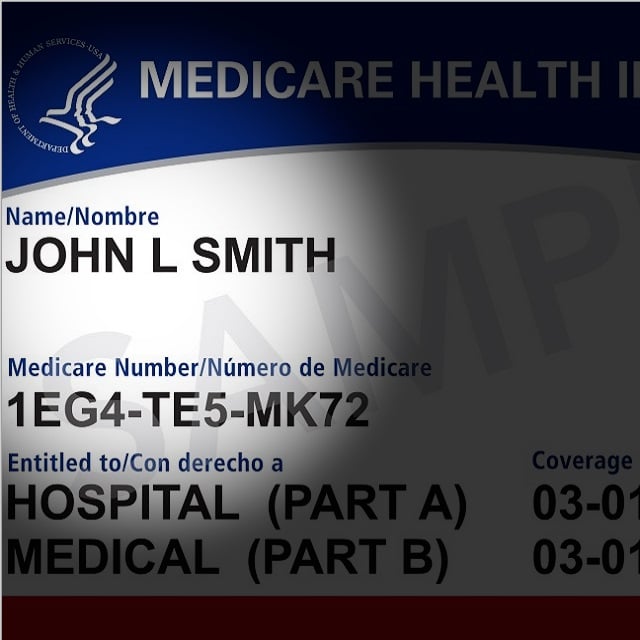
The backdrop: Medicare Advantage is a program shaped by Part C of the Social Security Administration section that governs the Medicare program.






