I’ve been informed my therapist could be committing insurance fraud, need help figuring out how to confirm this and navigate this situation?
To preface, I know next to nothing about how health insurance works. I’m still a dependent under my parents’ insurance, so when I have an appointment I pretty much just show the front desk my insurance card, pay the co-pay ,and don’t look into it further. So in a recent situation I’ve been dealing with, I’m extremely confused.
Last year, I started seeing an evaluation for ASD & ADHD. I got in touch with a counseling center who put me on a waitlist for a therapist who specializes in ASD. I emailed her and asked about how the evaluation process works, she said:
“The complete diagnostic evaluation for ASD will require 4 two-hour sessions on different days, so the insurance will cover some of the evaluation, and about 6-7 office hours to process the assessments and write the complete evaluation, which will have to also be on different days due to insurance rules. Adding the ADHD evaluation would add one more 2-hour session.”
We had our first telehealth appointment in August. She told me that she would be leaving the counseling center soon and starting a private practice and asked if I would still be interested in working with her. I agreed. Where it starts getting fuzzy is that the above email is the only thing in writing I have from her describing the evaluation process. I don’t know if any of it still applied after she left the previous practice.
Over the call, she told me that the process would be about 15 hours total (each hour being one session). She said that the evaluation was $1500, but after insurance it would only be about $500. I was thinking this cost covered the diagnostic evaluation, processing the assessments, and writing the evaluation. My reasoning for this was she said each session would run around $80-$100 (before insurance) which aligns to the evaluation costs. If it’s a 15 hour process, and each appointment is $100, that works out to $1500. This time around she said the ADHD evaluation was included. Upfront she told me that insurance companies often don’t over the cost of adult ASD assessments, and that insurance would cover more by the appointments being spread out as one-hour sessions. In ASD spaces online it’s often talked about how it’s kind of messed up that insurance plans tend to only cover ASD evaluations for children and not adults, so I was under the impression she was doing this because she agreed it was unfair and wanted to make the process less expensive for me. But originally, the reason was because of insurance rules so this is also confusing. She also said to bill my insurance company she needed to enter a diagnosis, so she said she was going to put it as GAD in the system. I don’t have GAD, it was just put there as a placeholder until I got my ASD & ADHD diagnoses I think.
Fast forward to now. I finished up the diagnostic evaluation process in October and had been waiting on her for the final report for several months (which is another story within itself). After several delays, last Tuesday (5/10) she finally texted me with an update that her plan was to send me the evaluation on 5/12. She said, “The remaining balance that the insurance did not cover is $475.39, which will be billed to your card you have on file once the evaluation is emailed to you.” I did not expect this charge. I was under the impression that the sessions I’d already paid for (through co-pays) towards the diagnostic process last year covered the entire process. So when I received this $475.39 fee, I was like, “Wait, is this the $500 she was talking about originally and I misunderstood?” I’ve been wondering if there’s some misunderstanding and if the report itself is a separate charge from the testing and I didn’t realize it. I did not respond to her message because since I’m not sure if it’s justified or accurate, so I didn’t want anything I said to be considered agreement.
Through talking to others about this I discovered my therapist didn’t communicate to me well. The process and billing wasn’t explained to me clearly, and the billing aspect should have been put in writing but it was not. It’s not even in the contracts. So that makes understanding this situation even more difficult.
I looked in my portal and saw an invoice has been issued 5/1 through my therapy portal listed as “ASD Assessment and Evaluation (ASDAE)” and the amount was $30. On 5/11 an invoice was issued as “Fee adjustment for the session on 5/1/22” and the amount was $475.39. Neither of these charges have appeared as claims on my insurance yet. I don’t know what that means or what to make of that.
According to the invoices stored in the portal, for most days of the assessment she billed them as psychotherapy. The codes from the dates of the assessments are:
8/19 – 90837, +90838
8/26 – Psychotherapy, 60 min (90837)
9/2 – Psychotherapy, 60 min (90837)
9/9 – Psychotherapy, 60 min (90837)
9/15 – Psychotherapy, 60 min (90837)
9/30 – 90837, +90838
9/15 – Psychotherapy, 60 min (90837)
9/30 – Psychotherapy, 60 min (90837)
10/3 – 90837, ASD101
10/10 – Psychotherapy, 60 min (90837)
3/3 – Psychotherapy, 60 min (90837)
I shared my experience online and have been informed that what she was doing may be insurance fraud or balance billing. They said I should review my EOBs to see if I was charged the correct amount. This is where I get extremely confused, because I’m not sure how to use the EOBs to interpret what’s going on here. According to the EOBs, it reflects that my copay has been $30 for previous appointments and I’ve paid all those so I’ve done my part. It still doesn’t really help with figuring out if I’ve been billed properly. I’m not sure what to make of the information or what to do next. They suggested I should call the insurance company and bring this up, but before I call and ask I feel like I need to have a fuller understanding of what I need to ask them and why I’m asking it, or I might not understand the answers they give. I’m not even sure what my insurance’s policy is for coverage of ASD & ADHD evals because I can’t find concrete information on MyUHC.
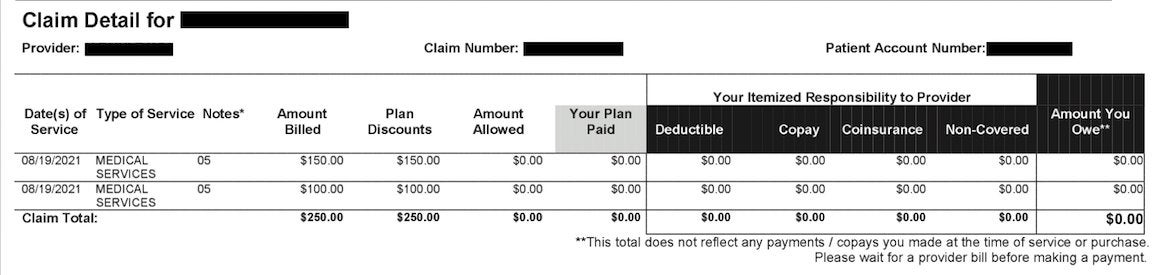
Other things that confuse me is that it looks for previous appointments like she has sent multiple claims for the same date and something went wrong with them. It looks like she would list multiple services under the same date but only one would go through. I’m not sure if the repeated claims are replacements to correct previous ones, or if she’s overcharging the insurance company. I have not had to pay extra for these. Here’s claims from 8/19 as an example: https://imgur.com/a/KvNhvek
Also, now I’m confused if the way I’ve been being billed for sessions is general is correct. Someone told me I should I always wait for it to go through insurance before I pay, but I’m not sure how to tell if it went through insurance first or not. This is how it typically works for my appointments with her. I see her through telehealth so all transactions are online. For all of my sessions, payment has automatically been charged to my card on file afterwards. E.g. for an appointment on 1/13:
On my bank statement the transaction name is “PAYMENT AUTHORIZED 1/13”, I assume this is when it started pending.
I got an invoice to my email marked “PAID” at 12:22 AM on 1/14.
The the claim was received by insurance 1/14, and processed 1/15.
The charge was posted to my bank account 1/18.
So it looks like for each appointment the money is charged to my credit card before the claim is received. I don’t know if the day a claim is received is the same as the day it’s sent. It looks like most claims were received the day after payment, sometimes the same day. I’m unclear on if this is supposed to be happening or not.
So the heart of the matter is that I’m trying to figure out whether this $475.389, and the individual charges for each session of the process, are unjustified or if this is technically accurate and she wasn’t clear with me about her service fees. I don’t know if she’s billing this way because she wanted to save me money on the evaluation process, or if there’s something suspect going here. If she was trying to do me a favor and save me money, I don’t want to rat her out. If the charges are unjustified though, I need to know that so I can go about seeing how I can get my money back. And I’m very confused about where to begin figuring out if these charges are justified or not. I don’t want to cause a stir or accuse her of anything until I can better understand this.
EDIT: Meant to add that she’s in-network.







