Impact of medication cost-sharing on adherence, clinical outcomes, health care utilization, and costs
This is the paraphrased title of a paper by Fusco et al. (2023). The authors conduct a systematic literature review of studies published between 2010 and 2020 and find that among the 79 articles screened:
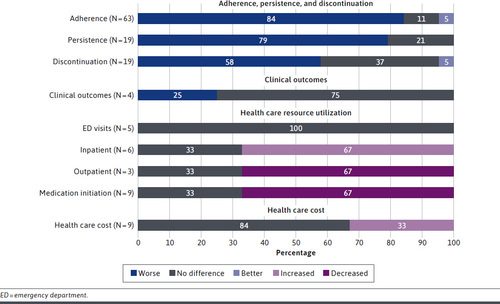
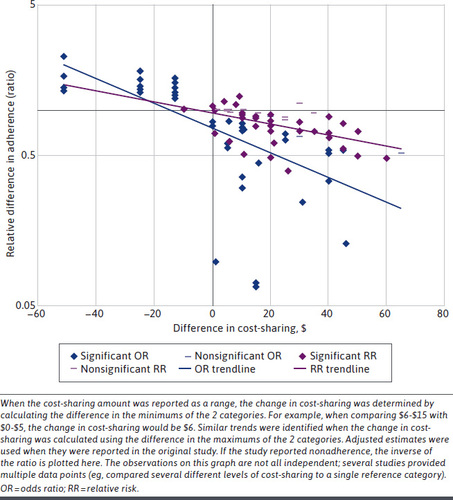
The majority of publications found that, regardless of disease area, increased cost-sharing was associated with worse adherence, persistence, or discontinuation. The aggregate data suggested the greater the magnitude of cost-sharing, the worse the adherence. Among studies examining clinical outcomes, cost-sharing was associated with worse outcomes in 1 study and the remaining 3 found no significant differences. Regarding HRU [healthcare resource utilization], higher-cost-sharing trended toward decreased outpatient and increased inpatient utilization. The available evidence suggested higher cost-sharing has an overall neutral to negative impact on total costs. Studies evaluating elimination of copays found either decreased or no impact in total costs.
There are two challenge with the paper (i) publication bias and (ii) cost sharing measurement. With respect to the former, are papers that show no relationship between cost sharing and adherence, HRU and cost less likely to be published? Potentially. While this bias likely would impact the point estimates, it seems logically and empirically very strong that higher cost sharing reduces adherence and increases inpatient admissions. Publication bias may be more influential for the other outcomes measured (i.e., clinical outcomes and cost). The second challenge is that cost sharing may be measured in different ways across studies. The authors do mention that the type and magnitude of cost sharing varied across studies. More importantly, however, the relationship between cost sharing and outcomes is difficult to estimate empirically since what one would like to measure is the cost sharing structure a patient faces; if you don’t fill a drug because cost sharing is too high, observed copayments in the data will be $0 but the true cost sharing one faces is large. On the other hand, if a person has low cost sharing, they may decide the fill the drug and observed cost sharing (as measured in claims) would be high even if the benefit design is very generous. Since claims data only include amounts paid rather than a patient’s benefit structure, creative econometric solutions–or data that combine claims and benefit design–are needed to estimate the relationship between cost sharing and cost in a more rigorous manner. Nevertheless, by conducting a systematic literature review of these studies, Fusco and co-authors have provided an important review for researchers to evaluate these issues for individual studies in more detail.







