How to manage food allergies

Russell Cain Updated: 30 January 2020
We live in an age of food panic. If you were to do look at your online search history, the words gluten free, diary free, soy, egg and/or nut free are most likely in your most recent searches. This is not surprising. According to the Centres of Disease Control and Prevention, food allergies among children have increased approximately 50% between 1997 and 2011.
Australia has one of the highest reported food allergy incidence rates in the world. An ASCIA â Access Economic Report estimated that in 2007, 19.6% of the Australian population had at least one allergic disease. Although most food allergies cause relatively mild and minor symptoms, some can cause severe reactions, and may even be life threatening. Are you prepared, do you have an allergy action plan?
Before you can create such plan, you need to know what it is, how it can be managed and if itâs preventable. This article aims to answer those questions and in so doing facilitating early recognition and control of the allergic disease.
What is a food allergy?
An allergy occurs when your bodyâs immune system overreacts to a food protein, sending out chemicals to defend itself, because it has mistaken that food protein as a threat.
âAllergyâ refers to conditions that involve changes to your immune system. These immune system changes fall into two categories:
1. Immunoglobulin E (IgE) mediates:
The symptoms are the result of interaction between the allergen and a type of antibody known as IgE, which is thought to play a major role in allergic reactions.
2. Non-IgE-mediated:
The symptoms are the result of interaction of the allergen with the immune system, but the interaction does not involve an IgE antibody?
Why you need to know the difference: The difference between IgE and non-IgE is important for when you are discussing allergy testing with your doctor.
IgE mediated reaction Non-IgE mediated reaction Food-specific IgE antibodies form and latch onto the bodyâs allergy cells Involves immune system T-cells, NOT IgE antibodies Immediate onset, but may be delayed up to 3 hours Delayed onset; hours or even days Triggers onset of allergic symptoms Disturbs the gastrointestinal tractSymptoms:SwellingHivesWatery/itchy nose or eyesDifficulty breathingTrouble swallowingVomitingSymptoms:Upset stomachVomitingDiarrheaBloody stools Anaphylaxis (severe allergic reaction, affecting the whole body) may occur No Anaphylaxis occurs
Whatâs the difference between a food allergy and food intolerance?
Food allergies involve your immune system and can be life threatening. A food intolerance is when your body has trouble digesting food. For example, if you are lactose intolerant, you are missing the enzyme that breaks down lactose, a sugar found in milk. So, if you were to drink a glass of milk or eat a slice of cheese you will likely experience bloating and nausea. On the other hand, if you have a diary allergy and you drink a glass of milk you could suffer a severe allergic reaction, i.e. breaking out in hives and/or having trouble breathing.
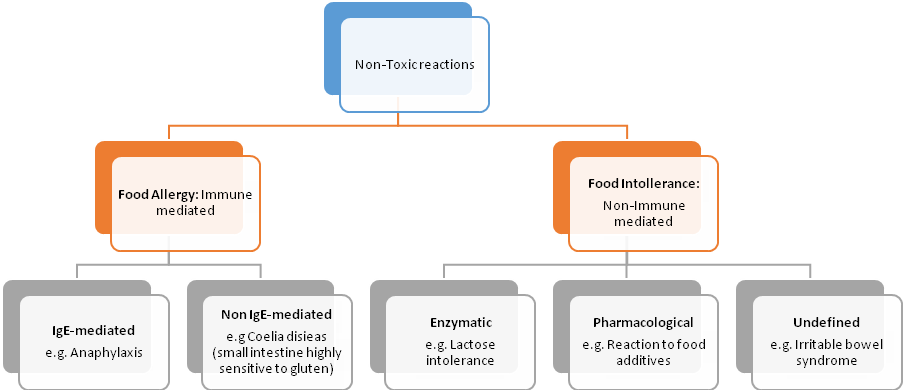
Adverse reactions to food can be further subdivided into non-toxic and toxic reactions. Toxic substances in food may affect any exposed individual, whereas non-toxic reactions are highly individual, and depend on genetic, epigenetic and environmental factors.
Non-Toxic reactions will be our focus
Most common food allergies
Food allergy occurs around 1 in 20 children and in about 2 in 100 adults. The foods which are commonly implicated in allergic reactions are:
For Children: Eggs, milk, wheat, soya and peanuts
Most food allergies start in childhood, but they can develop at any age. It isnât clear why, but some adults develop allergy to food they used to eat without a problem. Most people who develop adult-onset allergies usually do so in their twenties and thirties.
For Adults: Fish, shellfish, peanuts and tree nuts
Even trace amounts of a food allergen can cause a reaction in some people with food allergies. Although ingestion is the primary cause of severe reactions, in some cases, skin contact or breathing in a food protein can cause symptoms.
Can my food allergy be outgrown?
Most children eventually outgrow milk, egg, soy, and wheat allergies. Fewer outgrow peanut and tree nut allergies. Outgrowing a childhood allergy may occur as late as the teenage years. Food allergy that begin in adulthood tends to persist.
Diagnosis and Food Allergy Testing
The diagnosis of a food allergy will largely be based on your clinical history and physical examination. The natural history of a true food allergy is affected by the age at which it develops, the severity of the symptoms and the type of food implicated.
Be prepared to answer questions about:
What and how much you eat How long it takes for symptoms to develop What symptoms you experiences and how long they lasted
After taking your history, your allergist may order skin and/or blood tests:
Skin-prick test
Skin-prick test provide results in 20 minutes. The test is considered positive if a wheal (resembling the bump from a mosquito bite) develops at the site where the suspected allergen was place.
Blood tests
Blood tests measure the amount of IgE antibody to the specific food(s) being tested. The Radioallergosorbent test (RAST) is usually performed and results are generally available after a week.
If you suspect that either you or your child might have a food allergy, consult your family doctor or an allergist and avoid the substance or foods you suspect. The doctor will consider the diagnoses of a food allergy if:
You or your child is experiencing anaphylaxisYou or your child are experiencing a combination of symptoms within minutes to hours after eating food and/or after eating a specific food on more than one occasionYouâve been diagnosed with Eosinophilic Esophagitis (EoE); an immune/allergic condition that leads to inflammation or swelling of the oesophagusYour child has been diagnosed with severe eczema, EoE, enterocolitis, enteropathy, or allergic proctocolitis
Food allergy Action Plan
Prevention should start during the pregnancy stage. According to K. Grimshaw, Food Allergy Prevention Experimental Sciences, research has moved away from the avoidance of certain foods to the inclusion on specific foods into the diet. Maternal dietary factors that have been considered to have an impact on the allergic outcome of an infant are:
Polyunsaturated fatty acids. Babies born from mothers who had taken omega-3 supplements while pregnant had a decrease risk of developing food allergies and IgE-associated eczema. These âgoodâ fatty acids have anti-inflammatory properties and may modulate the immune response.Probiotics are live micro-organisms with various, strain-specific immunomodulatory effects which play an important role in the development of the mucosal and systemic immune system, specifically the development of oral tolerance.Folate. The human body requires folate to synthesise, repair and methylate DNA. Consequently it has been a nutrient of interest. Infant blood levels of the B vitamin between 50 and 75 nanomoles per litre were associated with the least allergic sensitisation in almost 500 children, according to the results published by Allergy.
The Australian Society of Clinical Immunology and Allergy (ASCIA) has developed information regarding infant feeding and allergy prevention. Their advice is as follows (use as a guide only):
Breastfeed for at least 6 months (if you are able)If complementary infant formula is required a standard cowâs milk infant formula may be used (where there is no history of allergic disease in the infantâs parents or siblings)If there is a history, the infant may be placed on a partially hydrolysed formula (Labelled âHAâ or hypo-allergenicSoy milk and other mammalian milk such as goatâs milk are NOT recommended for allergy preventionFrom 4 to 6 months, consider introducing a new food every 2-3 days. Introduce one new food at a time.
Allergy action plan: Management and Treatment
Not eating the allergenic food is currently the safest way to manage food allergy and prevent symptoms. You healthcare professional should work with you to decide whether certain related foods should also be avoided.
The food experts will offer tips for avoiding foods that trigger your allergies and will ensure that even if you exclude certain foods from your diet, you will still be getting all the nutrients you need.
You might want to consider going for training on how to understand ingredient lists on food labels and avoid products with warning labels such as âthis product may contain trace amounts of allergenâ.
There are drugs available that may prevent or decrease allergic reactions to food. However, they have side effects and in some cases can increase your risk of infection.
Conclusion
Knowing what a food allergy is and how it affects your body is a great start to beating the disease. Unfortunately, there is no cure and while you should remain vigilant of the foods you eat it is recommended you have a food allergy action plan in place.
As you get older food allergies are likely to take a toll on your health and familyâs finances. We recommend you review your insurance policies and make sure everything is in place should something unexpected occur.
Do you have an allergy action plan in place?






