How Friday Health Plans insolvency will affect policyholders in five states
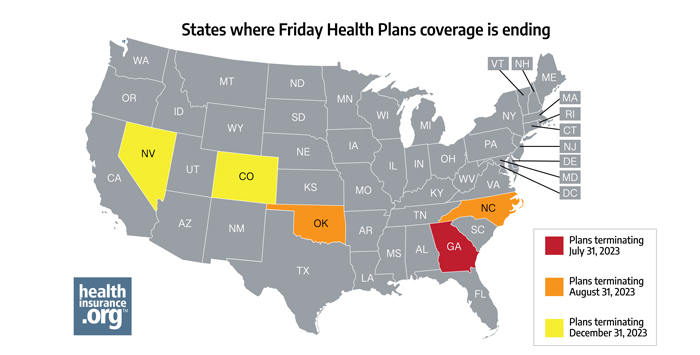
Friday Health Plans, which offers coverage in five states, is winding down its business operations. And in at least three of those states, thousands of enrollees need to select new plans in the coming weeks to avoid becoming uninsured.
Friday Health Plans of Georgia has been placed into receivership, and its health policies will terminate on July 31, 2023. Friday Health Plans of Oklahoma and Friday Health Plans of North Carolina have also been placed into receivership, with coverage ending on August 31, 2023. Enrollees will need to continue paying their Friday Health Plans premiums through those dates to maintain coverage until the plans terminate at the end of July or August, depending on the state.
Policyholders in these states will need to select new health insurance plans if they want to avoid coverage gaps for the remainder of 2023.
Learn more about what to do when your insurer stops offering coverage.
What is the deadline for Friday Health Plans policyholders to select new coverage in Georgia?
If you have Friday Health Plans coverage in Georgia, your policy’s coverage will end July 31, 2023. A special enrollment period for current enrollees began June 1 and continues through September 29.
To avoid a gap in coverage, you need to select a new plan by July 31. That will allow your new plan to take effect without a gap in coverage on August 1. If you wait until August or September to enroll, you’ll go a month or two without any insurance.
How will Friday Health Plans coverage termination affect customers in Oklahoma and North Carolina?
If you have Friday Health Plans coverage in Oklahoma or North Carolina, your policy will end August 31, 2023. A special enrollment period began July 2, and continues through October 30. To avoid a gap in coverage, you need to select a new plan by August 31.
(The special enrollment period runs for 60 days before and after the coverage termination date, which is why the windows don’t align precisely with the start and end of the calendar months.)
Automatic re-enrollment via the federal Marketplace (the exchange used in Georgia, Oklahoma, and North Carolina) is unavailable for mid-year plan terminations. So it’s essential for enrollees to select their own replacement coverage to avoid becoming uninsured.
To be eligible for subsidies, you must obtain your new plan through your state’s Marketplace / exchange. (Subsidized on-exchange enrollment and plan changes can also be made through an enhanced direct enrollment entity.) If you’re certain you aren’t interested in receiving subsidies, you can purchase new coverage directly from an insurer.
Will Friday Health Plans policyholders in Colorado and Nevada have a special enrollment period to buy new coverage?
If you have coverage with Friday Health Plans in Colorado or Nevada, note that no special enrollment period is set at this time. The current expectation is that coverage in Colorado and Nevada will end December 31 for enrollees who continue paying their premiums.
Friday Health Plans policyholders in Colorado and Nevada can select Marketplace plans for 2024 during the usual open enrollment period, which runs from November 1 through January 15 in both states. (A replacement plan will need to be selected by December 31 to take effect January 1.) If that changes, we’ll let you know on the healthinsurance.org website as the story develops. If a policyholder becomes eligible for employer-sponsored coverage, they will need to ask about the employer’s enrollment window.
What will happen to Friday Health Plans customers who have already paid out-of-pocket costs this year?
It is unlikely that your deductible and other out-of-pocket spending will transfer to new policies that take effect mid-year. People who have already paid out-of-pocket costs in 2023 under Friday Health Plans policies in Georgia, Oklahoma, and North Carolina will likely find they are starting over at $0 in out-of-pocket spending under their new policies. In Colorado and Nevada, the Friday Health Plans coverage is expected to continue through December 31. So out-of-pocket costs would reset to $0 on January 1 under a consumer’s replacement policy, just as they would on January 1 with any policy.
Louise Norris is an independent individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org since 2013. Her state health exchange updates are regularly cited by media who cover health reform and by other health insurance experts.







