Australia secures 450,000 new monkeypox vaccines. What are they and who can have them?
Health Minister Mark Butler today announced Australia had secured 450,000 doses of a third-generation monkeypox vaccine, 22,000 of which will arrive later this week.
There are now 58 people with the virus in Australia.
The announcement comes after the Chief Medical Officer declared monkeypox a “communicable disease incident of national significance” last week. This means the federal government can assist states and territories — for example, making antivirals or vaccines available through the national medical stockpile. It also signals the seriousness of the epidemic and the need to bring it under control.
Most of Australia’s cases are in New South Wales and Victoria, with most through travel, but some through community spread.
Globally, we have gone from a few hundred to more than 23,000 cases in three months, with the United States overtaking European countries to have the largest number of cases.
The epidemic is still largely spreading in communities of men who have sex with men, with over 98% of cases in this group.
Overseas, the rate of a concurrent sexually transmitted infection is around 30%, and HIV around 40%. The rate of HIV coinfection is much lower in Australia, reflecting the success in controlling HIV.
Read more:
Monkeypox in Australia: should you be worried? And who can get the vaccine?
What’s the new vaccine?
The third-generation non-replicating vaccine is the preferred vaccine for monkeypox. It has fewer risks of serious side effects than second-generation vaccines and can be given safely to people with weakened immune systems.
Australia hadn’t stockpiled these ahead of the epidemic, but the new announcement is a welcome move.
The vaccine Australia has just purchased is made by Danish biotech Bavarian Nordic. The only other non-replicating vaccine is the LC16m8 from Japan, and scaling up production is difficult, so supplies are limited.
Monkeypox is closely related to smallpox, and the smallpox vaccines protect against it and other orthopoxviruses. Smallpox vaccines are made from the vaccinia virus. First- and second-generation vaccines replicate in the body, so if someone is immunosuppressed, the vaccinia virus can spread and cause serious illness. These vaccines can also cause myocarditis and pericarditis in one out of every 175 vaccinated people as well as rarer serious side effects.
The first-generation vaccines such as Dryvax were used for smallpox eradication until 1980 when smallpox was declared eradicated, but had impurities because it was manufactured on the skin of calves.
The second-generation vaccines, such as ACAM2000, are made using cell cultures and are purified. However, these also replicate in the body and have the same side effects.
First- and second-generation vaccines are given as a single dose with a two-pronged needle that scratches the skin. A scar forms at the site, which indicates it has worked.
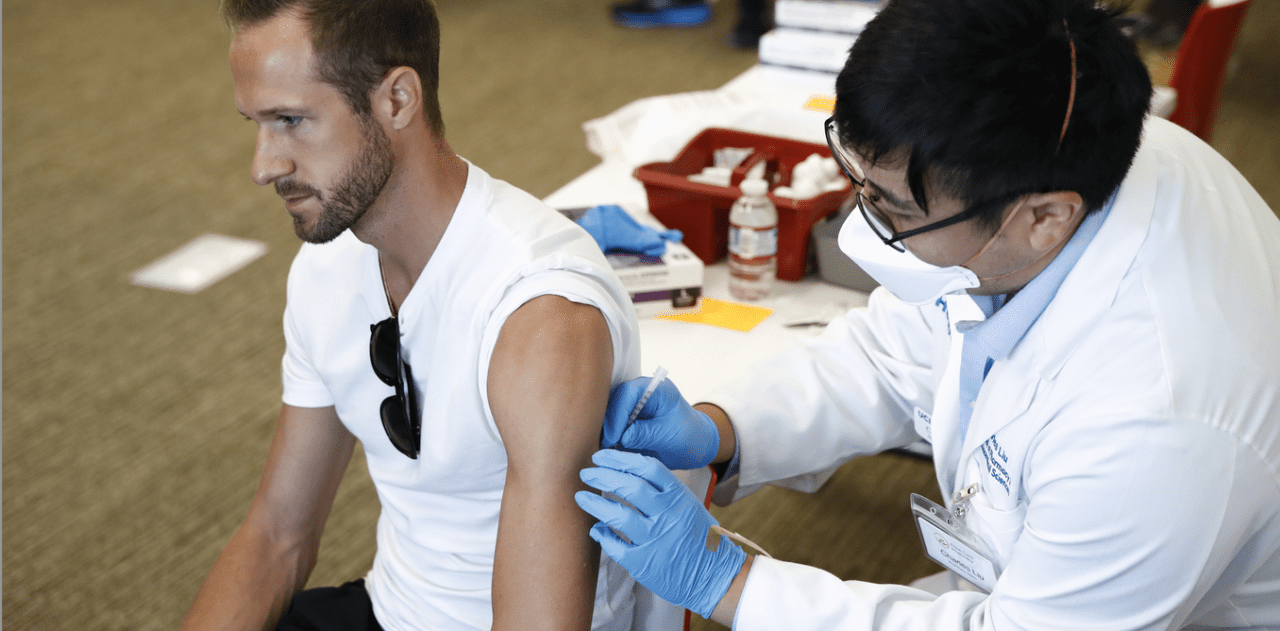
Third-generation vaccines need two doses and are given like other vaccines, and do not leave a scar.
Vaccine advisory body the Australian Technical Advisory Group on Immunisation (ATAGI) recommends the following people are prioritised for the vaccine:
high-risk monkeypox contacts in the past 14 days, including men who have sex with men who have recently had a high number of sexual partners or group sex, and those living with HIV
sex workers, particularly those with clients who are high-risk
anyone in the high-risk groups who is planning to travel to any country with a significant monkeypox outbreak.
Antivirals against smallpox (and monkeypox) were similarly not stockpiled ahead of the epidemic, but are expected to be available. There’s also a vaccinia immunoglobulin (antibody treatment) available to treat people with severe infection.
This outbreak is different
We don’t know much more about the genetic changes in the virus, except that there are more than 50 mutations. The virus appears to have been continuously mutating — and rapidly.
It’s possible some of these changes may be responsible for the rapid spread of the virus, and some new symptoms. Developing the rash around the genitals and anus is much more common in this outbreak than in the classic monkeypox presentation where the rash usually appears on the face, hands and feet.
A study from Cameroon found a 6% rate of asymptomatic infection. That’s not a high proportion, but shows that asymptomatic infection is possible. A pre-print study (not yet reviewed by other scientists) found that of 224 men screened, three had asymptomatic monkeypox.
Asymptomatic infection can also occur in vaccinated people, but none of the three men were vaccinated against smallpox. Still, this doesn’t adequately explain the spread of monkeypox globally.
Read more:
Monkeypox: an expert explains what gay and bisexual men need to know
So far the epidemic hasn’t spread widely outside of gay and bisexual men, and the death rate has been very low. Most deaths have been in children in countries in Africa where monkeypox is endemic. This means it is in the animal populations in those countries and causes outbreaks when infection spreads from animals to humans, and sometimes between humans.
To date there have been a handful of deaths in non-endemic countries such as Brazil, India and Spain.
Cases in children have occurred in the US and Europe. The risk of severe outcomes and death is much higher for children, so good outbreak control is important.
Australia should be able to control it
It’s important to ensure the virus doesn’t get established in animal hosts, which is a risk if the epidemic becomes very large. Rodents are the main host of this virus, but a range of other animals including monkeys can be a reservoir.
If the virus becomes established in animals in Australia, we will have to live with it forever – like we now have to live with Japanese encephalitis, which had never been found on the mainland until 2022.
It’s not yet known whether Australian native animals are susceptible to monkeypox. The virus is excreted in faeces, so environmental contamination poses a risk that the virus may get into waterways and thereby infect animals.
Read more:
Why declaring monkeypox a global health emergency is a preventative step — not a reason for panic
Australia should be able to control monkeypox, drawing on our successful HIV response.
This requires community engagement, good diagnosis, contact tracing and use of vaccines as both pre-exposure vaccine prophylaxis for people attending high-risk events or otherwise at high risk; and “post-exposure vaccine prophylaxis”, which you can take after you’ve been exposed to an infected person.







