At-Home COVID Tests: More Free Kits Coming, but How Many Will Insurance Cover? – CNET
Health insurance carriers are now covering a certain number of over-the-counter COVID tests per month.
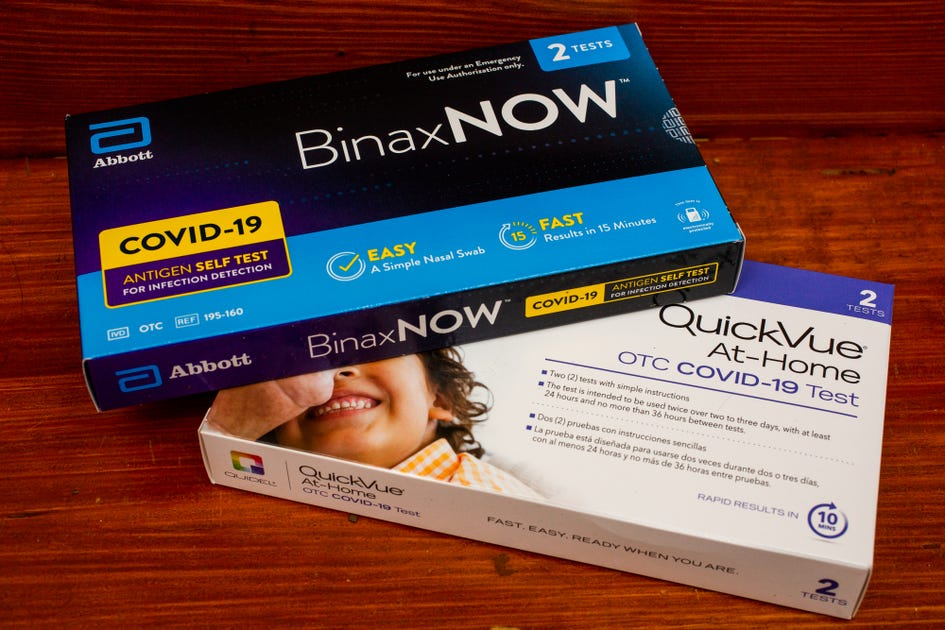
Sarah Tew/CNET
For the most up-to-date news and information about the coronavirus pandemic, visit the WHO and CDC websites.
If you’ve used all the free COVID-19 test kits you received last month, don’t worry: You can order more starting next week on the COVIDTests.gov website. If you need them sooner, COVID-19 test kits are also being covered by private health insurance companies. Plus, the government announced Medicare members will soon be able to be reimbursed for the over-the-counter diagnostics starting early spring.
Here’s everything you need to know about getting all the free at-home COVID-19 test kits your household needs. For more, get the latest on the best masks, how to pick the right booster shot and how to tell the difference between COVID, the flu and a cold.
Will my health insurance cover COVID test kits?
In January, the Biden administration mandated health insurance companies cover the cost of eight at-home antigen tests per month. If an individual has been directed to undergo COVID-19 testing by a medical provider because of underlying health conditions or other factors, there is no limit to the number of tests covered.
Get the CNET How To newsletter
Receive expert tips on using phones, computers, smart home gear and more. Delivered Tuesdays and Thursdays.
Though the Biden plan is not retroactive, some states — including Vermont — required insurers to start covering at-home kits earlier.
Carriers will typically front the cost at in-network pharmacies and reimburse members who buy them out-of-network. That reimbursement is capped at $12, so you may have to pay something depending on what test you buy and where.
You can find the full breakdown of how the insurance coverage and reimbursement process works here. Follow the links below for information about at-home COVID test reimbursement for the five US carriers with the largest memberships.
Several states are also issuing free COVID-19 tests to residents, including Colorado, Iowa, Connecticut, Washington, New Jersey, Maryland, Ohio, Oregon, Massachusetts and New Hampshire.
Washington, DC, is making at-home tests available for pickup at area libraries while other cities, such as New York and Boston, are distributing them to local health clinics.
You may also want to check with your employer, as some private companies are giving away tests and began reimbursing before Jan. 15.
How do I order free COVID-19 tests from the government?
All US households are eligible to request four free tests online at COVIDTests.gov or by calling 800-232-0233. If you already received the first round of tests, four more free tests will be available to order starting next week.
According to a White House statement, the US Postal Service is typically shipping these at-home tests within seven to 12 days of receiving an order.
In the continental US, the tests are being sent through First-Class Package Service, while shipments to Alaska, Hawaii, US territories and military addresses are being sent through Priority Mail.
Where can I buy at-home tests?
At-home rapid COVID-19 tests are available at pharmacies like Walgreens, Walmart, Rite Aid and CVS, and via online retailers like Amazon.
With the rise of the omicron variant in December and January, many pharmacies put caps on how many kits customers could buy. In early February, both Walgreens and CVS ended those limits.
How much do at-home tests cost?
Rapid antigen tests are generally much cheaper than home collection tests. Costs vary from brand to brand, but kits generally run about $10 to $25 apiece, with two tests per kit.
Both Walgreens and CVS are selling Abbott’s BinaxNow and Quidel’s QuickVue tests — two of the first authorized by the Food and Drug Administration — for $24 for a pack of two. Acon’s FlowFlex rapid test is currently $10 for one test at both Walgreens and CVS.
Home collection tests, which require a nasal swab or saliva sample to be sent to a lab for analysis, cost much more than the rapid antigen tests and require a much longer period to get results. But the “molecular” tests are considered far more accurate than antigen tests. CVS and Walgreens are selling Labcorp’s Pixel home-collection test for $125.
Do Medicaid and Medicare cover the cost of at-home test kits?
Medicare was not initially included in the White House’s insurance mandate for COVID tests. But the Centers for Medicare and Medicaid Services announced Feb. 3 that Medicare, which provides coverage to almost 63 million Americans, will start paying for eight home COVID tests a month in the early spring.
People with Medicare who also have private health insurance can receive reimbursement from their carrier now.
This is the first time that Medicare has covered an over-the-counter test at no cost to beneficiaries, according to the CMS, but members will still need to buy their tests at a participating pharmacy or retailer.
Medicaid already covers 100% of the cost of home COVID tests, as does the Children’s Health Insurance Program.
What if I don’t have health insurance?
For those without any coverage, Biden said there will be “thousands of locations” where you can pick up free COVID-19 test kits to use at home in private, rather than get swabbed in a drive-thru clinic.
Those who don’t have health insurance can also access free kits at community health clinics and other local sites. The HHS offers a search tool for finding community-based testing sites for COVID-19.
You can also order your free tests from the COVIDTests.gov website, though you’re limited to four per household.
Are at-home COVID tests accurate? Or should I get a PCR test?
There are two main types of COVID-19 tests: rapid antigen tests and polymerase chain reaction tests. Antigen tests can be taken at home and return results in about 10 to 15 minutes. PCR tests are more accurate but require lab work — and generally don’t provide results for at least 12 hours and sometimes up to five days.
Both tests typically use nasal swab samples, though some may collect saliva. PCR tests administered by a professional may require a nasopharyngeal sample that involves a much deeper nostril swab. Rapid antigen tests usually require swirling a swab in the nostril less than 1 inch deep.
PCR tests amplify genetic material from the collected sample up to a billion times to detect even the slightest amount of COVID-19 genes, making them highly accurate. They’re also more expensive and usually cost more than $100 apiece.
Rapid antigen tests simply detect the presence of COVID-19 antigens — the substances that prompt your immune system to create antibodies — and work much like home pregnancy tests. If your sample contains COVID-19 antigens, the thin line of SARS-CoV-2 antibodies on the test strip will change color.
Because rapid tests are simply looking for the existence of antigens, they work best when someone is symptomatic. Rapid antigen tests are less successful with early infections and asymptomatic cases. The risk of a false negative is much higher with a rapid test than a false positive.
The type of test you choose will mostly depend on your situation. Do you need results right now, and are you willing to risk less accuracy? Then rapid antigen fits the bill. If you want closer to 100% accuracy and don’t need instant results, the “gold standard” PCR is your best choice.

Watch this:
What to do if you lose your vaccination card, and how…
3:00
What if I test positive for COVID-19 using an at-home test?
If you take an at-home test and it’s positive for COVID-19, it’s recommended that you share the results with your medical provider and local health department. Methods of reporting self-tests to health departments vary wildly, though. Some have online forms, others require email and others use phone reporting. Check your local health department website for specific info on how to report a positive result.
After receiving a positive test result, you should isolate for at least five days, and longer if you’re symptomatic, according to the CDC. Though the risk of false positives from rapid tests is low, most medical experts and health officials still recommend confirming a positive at-home test with a subsequent PCR test.
For more information, here’s the latest on mask mandates and what scientists know about long COVID.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.







