Ambetter Illinois Refuses to Cover me despite paying and being eligable. Please give advice.
Hi, I’m looking to see if anyone has advice on what to do with my situation.
I moved to Chicago a couple of months ago for a new job and signed up with Ambetter. They were able to cover the meds I needed (to assist with my anxiety disorder) for the rest of 2022 and I didn’t have any problem with them. So during open enrollment I chose them again.
That all changed this year. I was supposed to have a doctor’s appointment in the middle of Jan but my insurance was suspended. Turned out an error on their end turned off the autopay, so I wasn’t able to pay the premium. I didn’t receive any notification about this error through a phone call, text, mail or email, and the website continued to throw an error every time I attempted to look at my billing information.
I called Ambetter Illinois and they said since I was unable to pay for January I would be uninsured for the rest of the month, but that I could pay for February. I attempted to get my bill paid for Feb because the site wasn’t working, but every single person was incredibly unhelpful. One said they were unable to get a way to bill me from the website and I couldn’t just tell them what my card was. Another said I had to wait two weeks for an audit to get my billing information in order to take the next steps which may take more additional weeks. Others said I was flat out screwed. I was given a million “sorrys” and zero helpfulness with what I was supposed to do. I was hung up on several times, transferred back and forth between departments over and over again, and had the most soulless apologies coming out of people who clearly did not care about my situation.
After calling them for I think the 16th time, I finally got someone to process my payment. I asked her, is there anything else I need to pay? She said for Feb, no. I asked her, on Feb 1st, would I be insured and she said yes, there is nothing more to worry about. In the meantime I’m unable to get my anxiety medication but I should be able to be fine off of it for the rest of the month and pick them up on the 1st. The medicine was over $1,000 uninsured, and I was only paying $40 per month for them.
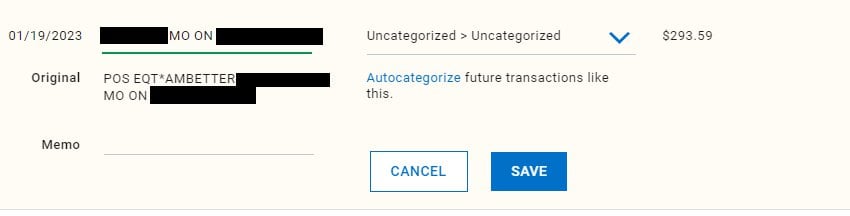
I scheduled another doctor appointment for Feb 1st but had to cancel again because of another insurance issue. I logged in and saw I was still suspended for an “outstanding balance”. I looked at the bills and they were charging me twice for January, a month I wasn’t even insured for, and once for this month. There was no record of me making a payment to them for Feb even though I see the charge on my bank account:
https://ibb.co/Kq7pW2m
The sum of the money they’re asking for is around $1,000, for absolutely nothing. Even if I was covered for January I shouldn’t be charged twice, but they refused to let me pay and get covered for January on every count back in the middle of January, so why am I being charged for it now that the month is over? Here’s more pictures from my billing page:
https://ibb.co/D8q0fc0
This mentions I owe money for January 2023 when I was not covered. The other mentions Feb 2023, yet I provided a picture that I already paid for that month. For February 2023, this is what the bill looks like:
https://ibb.co/TP867nP
Not only did I already pay for this month, but if you look at “Past Due” you’ll notice it matches the amount for this month and January. They are asking for both “Past Due” for January and the January bill itself, I am being charged $322.37 3 times. If the person on the phone made a mistake and I owed more for my premium (since I only paid $293.59) that’s fine and I will pay the difference. The next page claims I never paid for Feb and that my last payment was for December 2022 coverage:
https://ibb.co/P4w9FfX
The first payment was for December coverage. The previous was for November and October, failing to pay October on time was 100% my fault and I resolved it as I found out. Autopay was turned on and worked for the November payment, only to be turned off later, resolving in the beginning of this problem.
So I called again and was treated exactly the same. More waiting, more fake “sorry”s, more hang-ups and being transferred to departments a million times. I even had the case number from when I paid this amount over the phone but nobody could still help me. Lots of bad sounding telephones (which shouldn’t be a problem in 2023) and no help. I emailed them all of the evidence that I had, with no response. I’m still uninsured and off my meds and really frightened about that, and if something emergency level were to happen to me while uninsured.
So my question is, what do you suggest I do about this situation? Whether it’s a new approach or taking legal action. Or maybe I’m an idiot missing something super obvious and someone can correct me, but even then I don’t know why I’m being treated so poorly. My employer is aware of the situation and doing everything they possibly can to help with my situation.
I just want to be covered again, as I’m eligible and already paid to be covered. I am feeling the effects of withdraw from being able to get the medication I need to function. I do not consider this to be a complicated problem and I believe it could get resolved relatively quickly if somebody at the company cared enough. Thank you for you time.
– Adam







