His Anesthesia Provider Billed Medicare Late. He Got Sent to Collections for the $3,000 Tab.

Thomas Greene had been experiencing pain in his right leg, a complication from diabetes, when doctors recommended a procedure to increase blood flow to the limb.
Retired from a career as an electrician and HVAC technician, he had an outpatient procedure in April 2021 to alleviate his pain by dilating the clogged artery using a balloon snaked into his blood vessel.
Greene, who lives in Oxford, Pennsylvania, came through the procedure without any problems, and it reduced his discomfort, said his wife, Bluizer Greene. She spoke with KFF Health News on behalf of Greene, who is recovering from other health problems.
Greene is covered by Medicare and a supplemental policy through Humana and did not expect to pay anything for the care, Bluizer said.
Then the bills came.
The Patient: Thomas Greene, 74, who is covered by original Medicare and a Medicare supplement policy sold by Humana.
Medical Service: Peripheral artery bypass surgery on Greene’s right leg.
Service Provider: The operation was performed at Jennersville Hospital in West Grove, Pennsylvania, which closed in December 2021. Anesthesia services were provided by two providers who work for North American Partners in Anesthesia, which is private equity-owned and, with thousands of providers operating in 21 states, identifies itself as among the nation’s largest anesthesia staffing companies.
Total Bill: For the anesthesia care, North American Partners in Anesthesia billed $2,965.58: $1,334.51 for a certified nurse anesthetist and $1,631.07 for an anesthesiologist.
What Gives: North American Partners in Anesthesia, or NAPA, pursued Greene to pay for his anesthesia care instead of billing Medicare on time, sending the debt to collections before the couple discovered the problem.
Medicare eventually received the claims from NAPA, months after the couple started receiving collection letters, Bluizer said. But Medicare denied them because they were filed late — nearly 17 months after the surgery. Humana also denied the claims.
Medicare requires providers to submit claims within a year of providing their services. And Medicare supplemental policies, like Greene’s plan from Humana, generally do not pay for services if Medicare doesn’t cover them, whether because Medicare has not paid its part yet or because the program denied the claim.
Email Sign-Up
A year after Greene’s surgery, in spring 2022, the couple opened a letter from a collection agency working on behalf of the anesthesia group. It demanded Greene pay about $3,000.
“Something has to be wrong, because this is the first time my husband has ever been asked to pay out-of-pocket and we’ve had the same insurance for years,” Bluizer said.
She said for several months she called NAPA and the collection agency, C.tech Collections, of Mount Sinai, New York, to determine why it was billing her husband.
Greene was also contacted by the Faloni Law Group, a second organization working on behalf of NAPA to collect the debt, and Bluizer said she followed its instructions to respond by mail, disputing the debt on the grounds that it should be billed to insurance.
But her communication attempts did not resolve the issue, and she said her husband continued to receive collection notices.
Neither debt collector responded to requests for comment.
Bluizer Greene works at home in Oxford, Pennsylvania. Greene contacted the anesthesia staffing company and two debt collectors to determine why her husband was billed for anesthesia services the couple expected Medicare to cover.(Rosem Morton for KFF Health News)
“We were angry, and it was very upsetting because we had never had a bill put into a collection agency for any of his hospitalizations, and it was money we did not feel that we owed,” Bluizer said.
She said they may have received some letters from the anesthesia group in 2021 and 2022 that they discarded without opening because they believed her husband’s medical bills would be covered by insurance, as the rest of his surgery bills were.
Worried about the situation, including its potential impact on their credit, the couple reached out late last year to Harold Ting, a volunteer counselor for Pennsylvania’s MEDI program, which provides free assistance to Medicare beneficiaries. Medicare generally covers anesthesia services.
“This is totally unfair that a beneficiary ends up having to pay for what should be a totally covered service, when the provider is at fault,” Ting said.
Two explanation of benefits statements from Humana show the insurer received claims from NAPA in April 2021, shortly after Greene’s surgery. The statements said the claims could not be considered at that time, though, because Humana had not yet received Medicare EOBs for the services.
Kelli LeGaspi, a Humana spokesperson, declined to comment on Greene’s case. She said a Medicare EOB — a coverage statement generated when the program processes a claim — is required for the supplement carrier to consider a claim. Without it, a claim for secondary coverage cannot be considered and is denied, she said.
Supplement plans deny claims for benefits that are denied by Medicare, she said.
“If Original Medicare declines to pay the claim, then the Medicare supplement plan is required to decline the claim as well,” she said in an email.
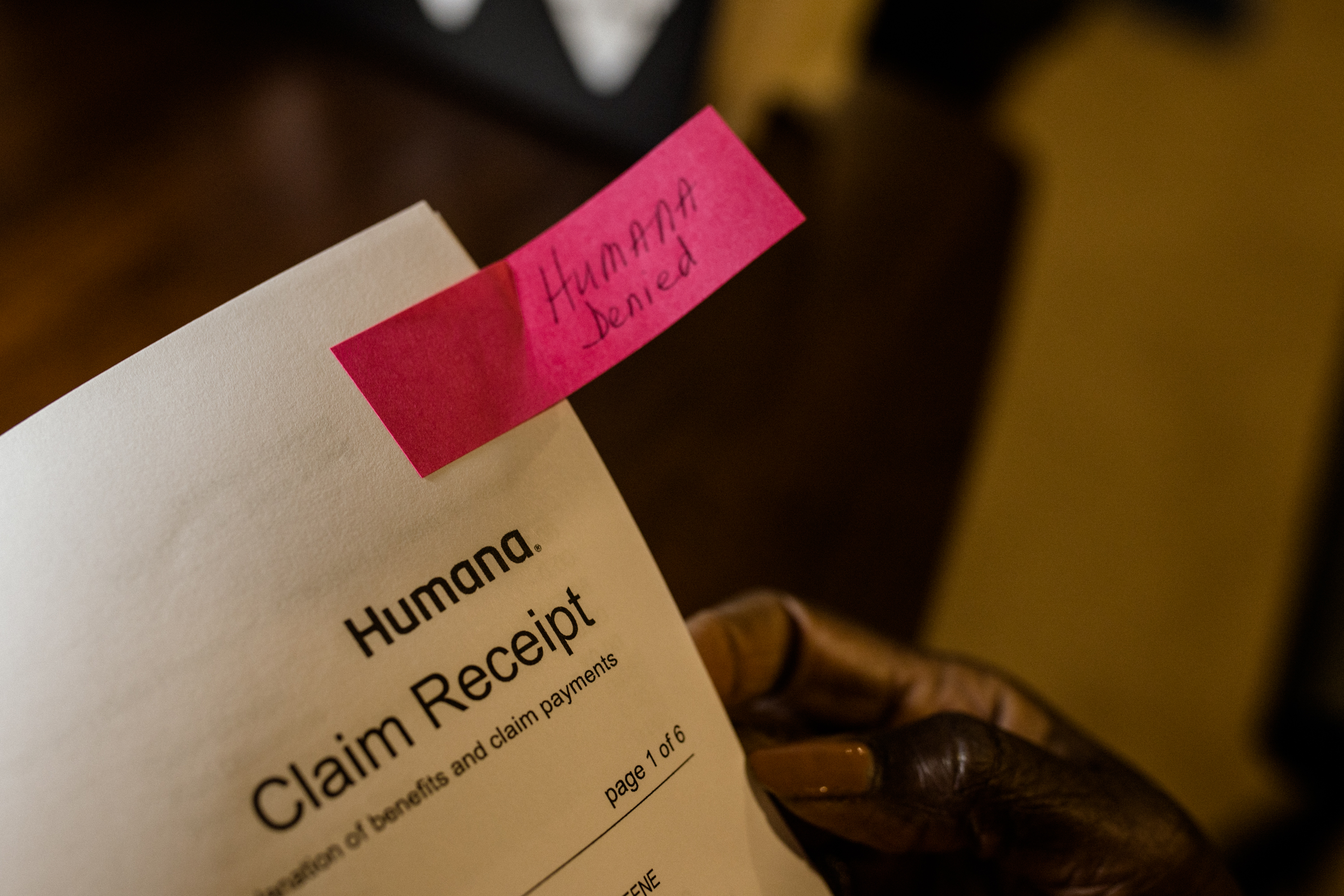 Humana, Thomas Greene’s Medicare supplemental insurance provider, denied claims for his anesthesiology bill because Medicare had not yet reviewed — or, it turned out, received — them.(Rosem Morton for KFF Health News)
Humana, Thomas Greene’s Medicare supplemental insurance provider, denied claims for his anesthesiology bill because Medicare had not yet reviewed — or, it turned out, received — them.(Rosem Morton for KFF Health News)
In December 2022, a NAPA representative told Bluizer in an email that NAPA billed Medicare after the April 2021 surgery and that Medicare denied the claims in August 2021. The representative provided an account statement showing the claims were sent to collections that month.
But Bluizer said a Medicare representative told her in late 2021 that the program had received no claims from NAPA.
Greene’s Medicare account shows NAPA filed claims in September 2022, about 17 months after his surgery and about five months after he received his first collection letter. Both claims were denied.
A quarterly summary notice said while the time limit for filing the claims had expired, Greene also could not be billed.
Meena Seshamani, director of the federal Center for Medicare, said in an email to KFF Health News that if a Medicare provider sends a claim a year or more after a service is provided, it is denied except in very rare circumstances.
There is no exception for provider error, she said.
A spokesperson for NAPA declined to be interviewed on the record, despite receiving a signed release waiving federal privacy protections.
Martine G. Brousse, a billing expert and founder of the patient advocacy firm AdviMedPRO, said Greene’s Medicare notice should have reassured the couple that he did not owe anything, despite the several overdue-bill notices they received.
If the Medicare statement “shows a zero balance to the member, then the provider cannot legally go after the patient,” said Brousse, who is not involved in Greene’s case. “The patient has zero liability because it is not their fault” the provider billed Medicare a year after the surgery. “That is the end of the story.”
Another mystery about the claim is why NAPA billed separately for a nurse anesthetist and an anesthesiologist. Bluizer said her husband was not told why NAPA billed individually for the two medical professionals — a practice some insurers believe constitutes double billing.
Brousse said there could be a simple explanation, such as if the nurse anesthetist started the procedure and the anesthesiologist finished it or if the company charged for the anesthesiologist to work in a supervisory role.
But the Medicare claims document shows each provider billed for the same amount of time — a little over an hour.
“As far as I can tell, this looks like two providers billed with the same ‘I did the job’ Medicare procedure code,” she said. “Medicare cannot accept that without an explanation.”

Thomas Greene underwent a procedure to increase blood flow to his leg at a Pennsylvania hospital. The anesthesiologists were late in billing Medicare, and the debt went to collections before he and his wife became aware of the issue. (Rosem Morton for KFF Health News)

Bluizer Greene takes care of her husband, Thomas, who is recovering from health problems. The couple received multiple collection notices while she tried to dispute some of her husband’s hospital bills, which they had expected to be billed to Medicare. (Rosem Morton for KFF Health News)
The Resolution: Unable to get answers, Ting connected Greene to the nonprofit, Pennsylvania-based Center for Advocacy for the Rights and Interests of Elders.
In March, Ariel Rabinovic, an advocate with the center, contacted NAPA on Greene’s behalf and explained that federal law does not allow the group to bill Medicare patients for services Medicare does not cover. He said he was told the company would stop billing Greene.
Bluizer said the couple has not received any collection notices since then.
Rabinovic said he has seen other situations in which health providers who agree to accept Medicare try to bill patients for services Medicare does not cover, which is not allowed.
“Older folks have a lot of things going on, and dealing with this can be very confusing for them,” he said. “A lot of people end up paying because they don’t want to deal with it.”
Greene has faced several health issues and spent time in a rehabilitation hospital this winter. His wife said she was happy the billing issue had been resolved without their having to pay anything.
The Takeaway: When a Medicare statement says the patient may not be billed anything for a health service, that’s the bottom line. Don’t write a check, but also don’t ignore bills and collection notices, because they could ultimately hurt your credit.
Read your mail, the experts said. While Greene was not responsible for paying the anesthesia bill given that Medicare said he did not owe anything, the couple may have prevented the debt from being sent to collections if they had responded to the anesthesia group’s communications and confirmed it had Greene’s insurance information, Brousse said.
Keep copies of bills and insurance statements, especially Medicare EOB documents, or follow them on an online portal.
The couple was smart to reach out to advocates for help resolving the issue when they could not do so on their own, Rabinovic said.
“This is why people need to read their notices from Medicare even when it says ‘This is not a bill,’” he said.
Also, when an anesthesia bill includes charges for both a nurse anesthetist and an anesthesiologist, question the charges. Many insurers will not pay for both.
The Centers for Medicare & Medicaid Services recommend beneficiaries call 800-MEDICARE with questions about their care or bills or file a complaint online.
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
pgalewitz@kff.org,
@philgalewitz
Related Topics
Contact Us
Submit a Story Tip







