There’s no cure for sickle cell disease, but spotting it early can improve treatment
Most of the global cases of sickle cell disease are diagnosed in African countries. The Economist Intelligence Unit – the research and analysis division of the Economist media group – estimated that in 2020 the total annual cost of treatment and impact on the economy of sickle cell disease across sub-Saharan Africa was US$9.1 billion. This was expected to rise to US$10.2 billion by 2030. The Conversation Africa’s Ina Skosana spoke to Yvonne Dei-Adomakoh, director of the Ghana Institute of Clinical Genetics (Adult Sickle Cell Clinic), and Head of the Department of Haematology, University of Ghana Medical School /Korle-Bu Teaching Hospital to find out more about this condition.
What is sickle cell disease?
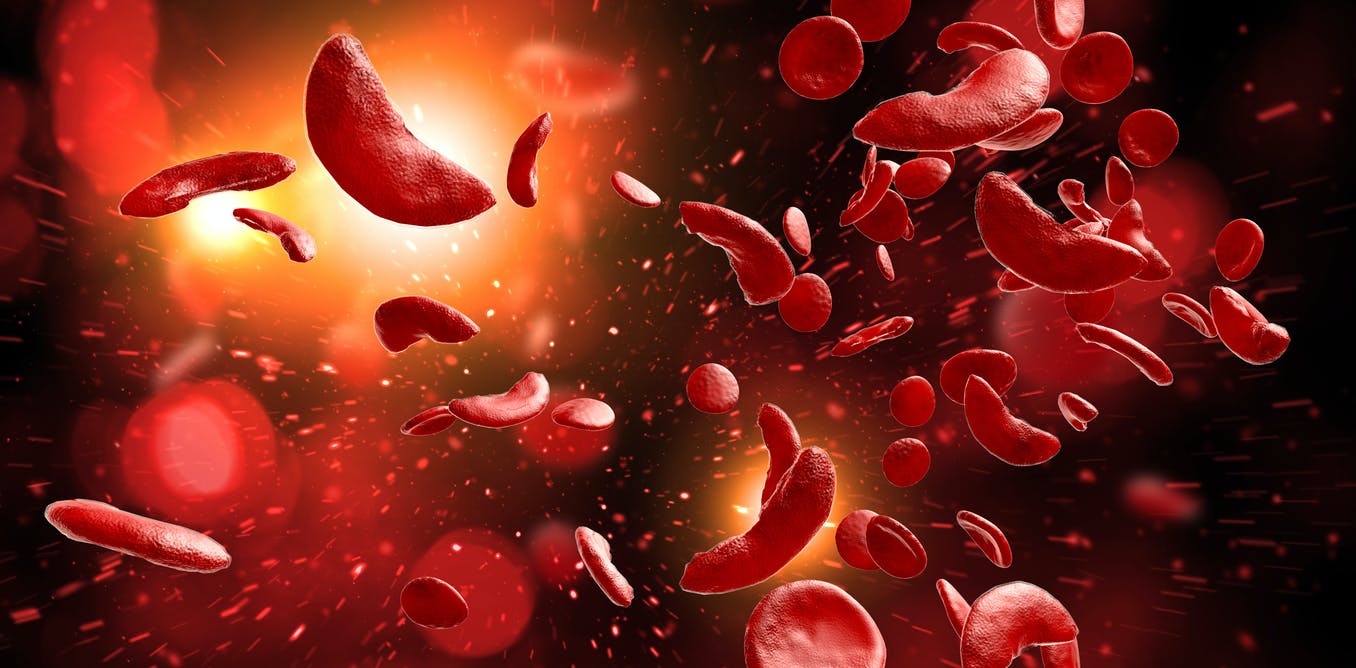
Sickle cell disease is a genetic disorder that causes misshapen red blood cells to clog blood vessels. The condition can cause extreme pain. People with sickle cell disease are at risk of life-threatening infections. These include pneumonia and meningitis. They are also at risk of other complications such as stroke or loss of vision. If left untreated, sickle cell disease can prove fatal. As a genetic condition, the disease is not preventable. But it can be managed with the proper treatment. Treatment is more effective if the disease is detected early in life.
The disease is a consequence of a gene mutation that granted a degree of protection against the threat of malaria. Research suggests the mutation originated in a single child in Africa roughly 7,300 years ago. It’s thought that the gene could limit the ability of the malaria parasite to infect host cells. The descendants of this child, with a greater resistance to malaria than those without the sickle cell trait, spread across the globe. Today, people with the gene are found in greater numbers in areas prone to malaria, such as sub-Saharan Africa.
When two individuals with the mutation pass copies of the gene to their child, the child will have sickle cell disease rather than sickle cell trait, and will not have the same resistance to malaria.
Those with the disorder are actually at higher risk of severe illness if admitted to hospital for malaria today.
How big is sickle cell disease in Africa?
An estimated 20 million people live with sickle cell disease globally. More than 66% of them are in sub-Saharan Africa. Around 300,000 children are born with sickle cell disease globally every year. Three out of four of these children are born in a geographic belt from Senegal to Madagascar – translating to 1%-3% of children born in this belt. Countries in Africa with the highest prevalence are Cameroon, Nigeria, the Democratic Republic of Congo and Ghana.
What measures are in place to manage it?
Just a few short decades ago, it was common for children with undiagnosed sickle cell disease to die from severe infections. But these cases are reducing with improvements in research and science. Newborn screening is preferable to testing following symptoms.
Early diagnosis, preventive care and active clinical management can prevent complications and death, and improve quality of life. If we know a child has sickle cell disease right from birth, we can put in place measures such as prophylaxis (screening for stroke or silent brain infarcts and starting disease modifying drugs such as hydroxyurea,annual assessment of organ function (liver and kidneys) and use antibiotics when required to ensure that severe infectious diseases do not occur.
Screening should be routine, because many children with sickle cell disease miss vital parts of their education.
Surveillance is conducted routinely in countries like the US, the UK and Jamaica, which have the infrastructure and resources to perform the screening.
A few countries in Africa, such as Ghana and Uganda, have adopted routine surveillance programmes. My research group and colleagues have demonstrated that routine newborn screening is possible and can be done in a cost effective manner with rapid and accurate results. Affordable paper-based point of care Hb electrophoresis would allow this even where resources are limited.
There has been a public-private-civil society partnership in Ghana since 2019. The Africa Sickle Cell Disease programme is a collaboration between the Ministry of Health of Ghana, the Ghana Health Service, the Sickle Cell Foundation of Ghana and the global medicines company Novartis. It has 59,121 babies currently registered and 24 health facilities involved. Newborns are screened and if sickle cell disease is detected, there is provision for follow-up. An app records patient treatment and experiences to build a profile of the patient. Data from laboratory tests are immediately shared with the app. Health workers can track progress more effectively, resulting in higher quality of care and faster time to treatment.
Partnerships like these use data and cutting-edge technology to allocate resources. They can improve the standard of care and address infrastructural gaps that may hinder the impact of healthcare in some areas. Because sickle cell disease management is complex, it requires partnerships for long term and sustainable projects.
What is the treatment?
We can’t yet cure sickle cell disease but we can manage the symptoms if we adapt the way we diagnose and treat it. Although it requires only a simple blood test, there was often little urgency about screening and diagnosis in the past, even among medical professionals, because care was simply supportive.
Effective treatment has considerably increased the chances of survival for those living with the condition. Since the turn of the century, we have used a medication called hydroxyurea to treat sickle cell disease. A formulation of hydroxyurea which is more suitable for young children will soon be available.
A clinical trial is under way in Ghana for a new treatment for sickle cell disease, crizanlizumab. This medicine is already available in Europe and the US.
Our study shows that an 89% decrease in maternal mortality rates can be achieved with a multidisciplinary care approach through pregnancy. Women with the disease have a higher risk of maternal mortality.
Developing knowledge and training medical staff on standardised practices for treating sickle cell disease has also been shown to be effective in reducing mortality.







