Medicare Agents Face Signs of Gloom
What You Need to Know
The GoHealth CEO said weeks ago that he knew big changes were coming.
Some midsize Medicare plan brokers have already dropped out of the market.
The turmoil could make this a good time for agents who are still in the game to increase market share.
Agents are getting signs that the annual enrollment period for Medicare Advantage and Medicare Part D drug plans for 2025 will be as stormy as insurers and big brokers had predicted.
Executives from CVS Health’s Aetna unit said during a conference call earlier this month that the company expected to let Medicare Advantage plan enrollment fall about 10% because of concerns about the effects of tight federal funding and new prescription drug benefits design rules on plan performance.
Elevance executives emphasized “disciplined” Medicare Advantage plan pricing, “efforts to recover margin” and the need for a “thoughtful and rational” strategy.
Executives from Centene talked about decisions to streamline their Medicare plan book.
Now, agents are talking about receiving warnings that Aetna is eliminating thousands of drug plans and, in at least some markets, may focus on offering drug plans that pay no sales commissions.
WellCare has announced plans to eliminate Medicare drug plan commissions.
Blue Cross Blue Shield of Kansas City is pulling out of the Medicare Advantage plan market.
What it means: Any agents or advisors with clients who have Medicare coverage need to be prepared to help them understand what’s happening and help them find the best available coverage options.
For agents in the Medicare plan market, the 2025 annual enrollment period could be a good time to increase market share.
The annual enrollment period: The upcoming Medicare plan annual enrollment period is set to run from Oct. 15 through Dec. 7.
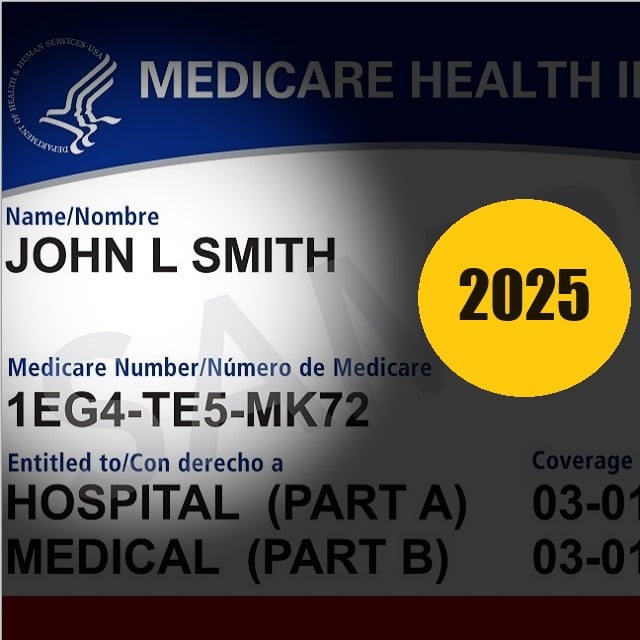
Most U.S. residents get a one-time initial enrollment period for the original Medicare Part A inpatient hospitalization program, the Medicare Part B outpatient care and physician services program, and the Medicare Advantage, Medicare Part D drug plan and Medicare supplement insurance programs when they turn 65.
The annual enrollment period affects people with Medicare Advantage and Medicare drug plans who want to change plans.
It does not affect consumers who are aging into Medicare eligibility or who want to sign up for Medicare supplement insurance coverage at any age.
What the GoHealth CEO said: Vijay Kotte, the chief executive of GoHealth, a Medicare plan broker, talked about the coming turmoil during a conference call with securities analysts in early August.
Health insurers gave clear signs of significant benefit disruptions, and there are signs that prices for plans that help pay the original Medicare program’s many out-of-pocket expenses could rise about 20%, Kotte said.
“We believe these rate increases and disruptions could lead to a significant increase in consumer shopping and switching during the upcoming AEP,” Kotte said.






