7 Questions about Commercial Health Care Prices
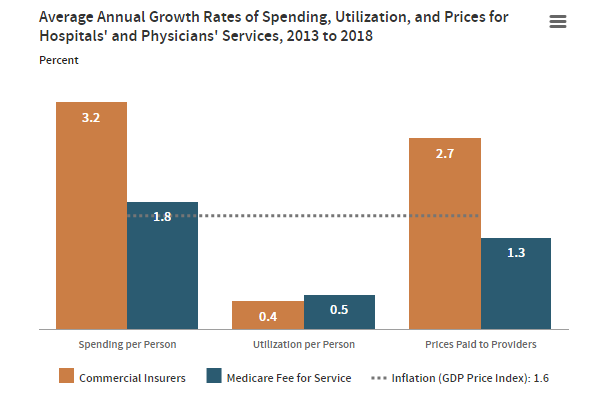
According to a 2022 CBO report, healthcare spending per person is much higher for commercially insured individuals than those insured by Medicare and this difference is largely drive by price differentials.
https://www.cbo.gov/publication/57422
Why are the outstanding research questions related to the prices commercial insurers pay providers? That is the topic of a recent Health Affairs article by Chernew and Berquist. According to that article, the key questions are:
Do Poorly Set Public Prices Distort Commercial Prices? If public prices are set too low, there could be cost shifting leading to higher commercial prices. On the other hand, if public prices are high, that could give health systems more leverage to negotiate higher prices for commercial insurers. The converse could be true for both. The market dynamics are complex and may vary across markets.How Should Services Be Defined? Typically this is done at a granular level (e.g., CPT codes, DRG codes). The authors write that “Detailed service definitions can help ensure minimal variation in delivery costs within any given service category. However, having many codes creates opportunities for providers to choose more lucrative codes. The sheer number of codes and continual updating of code definitions generates administrative costs.” The authors pose that maybe more general service codes may be more useful for getting providers to be more efficient. At the same time, these broader codes, would incentivize skimping on care, and decrease incentives to adopt innovative new techniques and services that could improve patient health. How Does Quality Respond To Changes In Pricing? The authors note that there is evidence suggesting that patients receiving care from more expensive providers receive better care; cross-national studies, however, show that price and quality are not always linked. Can we reduce price and maintain quality? The authors make an important point: “the relationship between price and quality may not be linear, and reductions in the price of high-priced providers may have a different effect than reductions in the price of low-price providers…[also] quality is multidimensional and different people may weigh different dimensions differently, making broad conclusions elusive ” How Should We Price New Digital Services? A key question is whether digital technologies are complements are substitutes for “analog” care. For instance, telemedicine visits may be able to substitute for in-person care in many cases. On the other hand, the ability to email your provider may improve patient satisfaction and quality, but paying for email responses from physicians likely would increase cost as it is a complement to analog services. How Much Spending Is Flowing Outside Of The Claims System? While claims data can help measure overall cost, much or payer reimbursement to providers comes through alternative payment model mechanisms such as shared savings payments, Hospital Readmission Reduction Program (HRRP) bonuses, and other value-based payments are not captured in claims. According to HCP-LAN’s 2022 report, only 40.5% of services are paid via standard fee-for-service (FFS); the other 59.5% are paid based on value or via capitation, bundles or global budgets. Are Pay For Performance Systems Worth It? Much of the Affordable Care Act provisions aimed to link reimbursement to quality through pay for performance (P4P). However, there is a growing body of evidence that quality doesn’t improve with P4P systems. Plus these programs add administrative cost and complexity for providers. Paying for value is good in theory; but is it feasible to measure quality in a valid way in the real-world and link to reimbursement in a manner that is not burdensome to payers, providers and patients? To What Extent Do High Prices Reflect Higher Costs Of Production In The US, And Why? Wage costs are higher in the US than other countries which explains some of this difference. Further prices paid for drugs and diagnostics are also higher. The US health care system multiple stakeholders add complexity and administrative costs. What other reasons are there for the higher costs of health care in the US?
You can read the full article here. The article concludes by noting that any policy option will involve tradeoffs between between spending, access, and quality. There is no silver bullet, but we can keep working towards making health care in the US and globally better for patients.







